“MY LACK OF MOTIVATION WAS PROBABLY THE MAJOR FACTOR.“
Q: What was your least favorite part of of rehab and what was the best part the rehab process?
A: The least favorite part was moving from body weight to added weight, transition was painful. Most favorite was getting to use the ice machine after workouts.
Q: Did pain influence your workout regime?
A: yes as soon is it became painful i would basically stop preforming my exercises. If the pain was manageable I would continue to work through the discomfort. Noted that under physical therapist supervision he pushed harder than when left to workout on his own initiative.
Q: What motivated you to workout at home when you didn’t have the therapist guiding your therapy?
A: For my first surgery in high school my main motivation was returning to the football field as quickly as possible. The most recent surgery i had less motivation to spend time focusing on strength training. Main motivation was the avoidance of pain, i just wanted to be able to sleep correctly at night.
Q: Was there a specific process during rehab that motivated your rehab workouts?
A: The most recent surgery, no. During the first one there was an electrical stimulation machine that helped relive pain, I looked forward to using that machine during each session after each workout session.
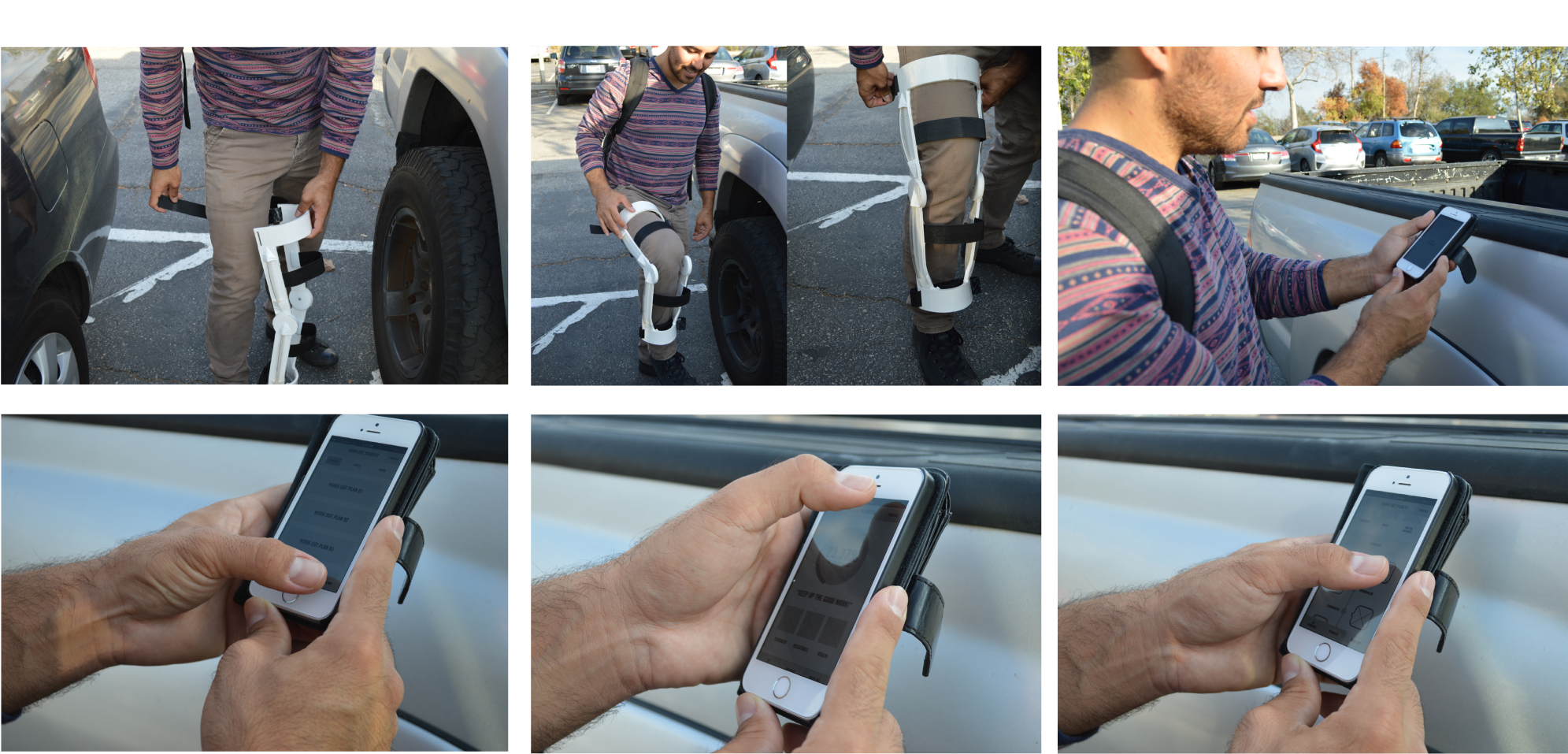
Q: Do you think the use of a physical therapist helped shorten your recovery process.
A: At home, there is less focus on recovery, with the physical therapist there it, motivated you to push harder than you would otherwise. I think part of it is the security of knowing that even if it does hurt, the therapist is there to let me know if in over doing it.
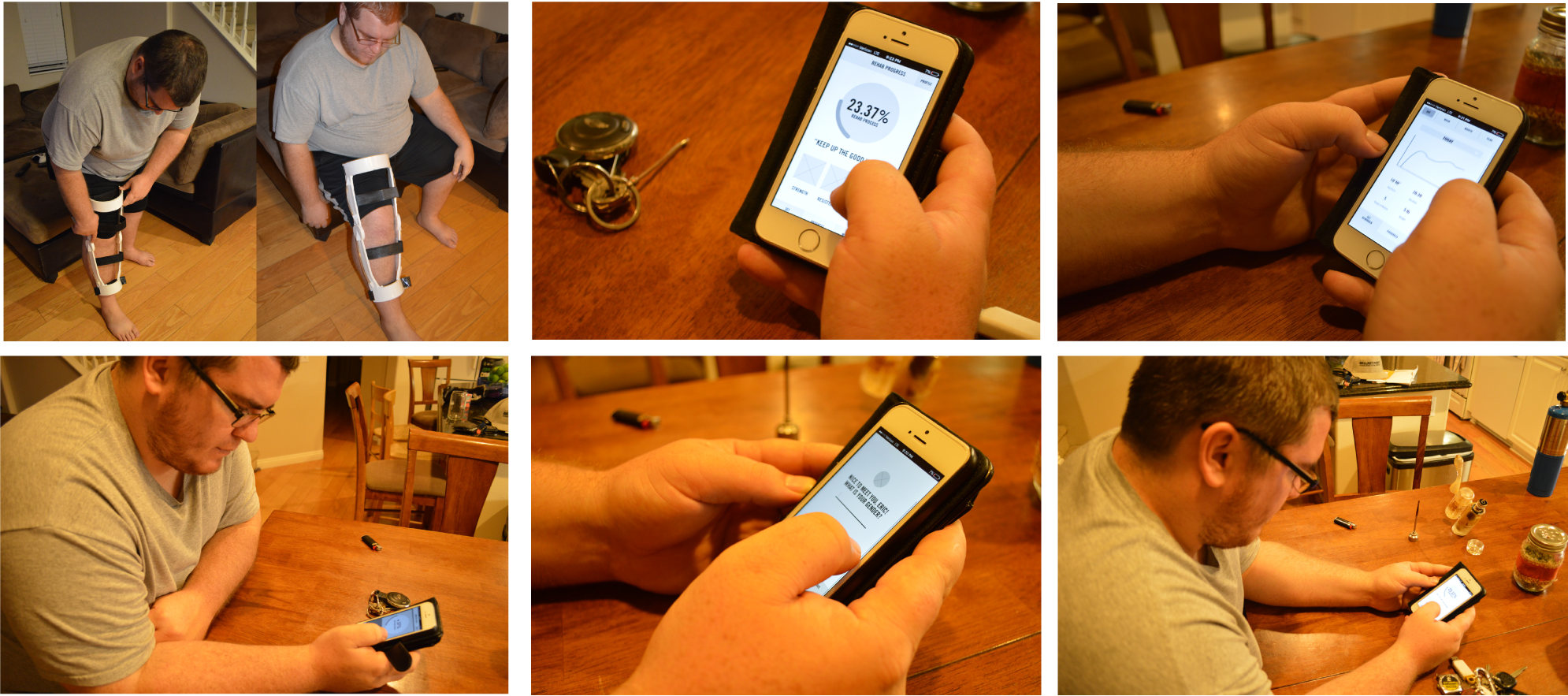
Q: Was it difficult to track your progress through rehabilitation?
A: Was difficult to gauge, main indicator was how much arm motion i gained and if something hurt significantly i just wouldn’t do it again. However, my therapist was highly aware of what different locations of pain indicated, even when i forgot to bring up incidents like rolling over during sleep, he was able to identify that i had done so without me saying so.
Q: Did any external factors play into your recovery process outside of doctors orders.
A: I lifted a bunch of things that i probably should not have done, however i do feel it helped me recover faster simply from an excessive stand point.
Q: Did pain play a factor on your willingness to participate in rehab.
A: Yes when pain reached a certain point i would stop therapy for the day. Pain kept me from following my doctors recommendations at home.
Q: Did you have a positive or negative attitude towards your recovery and rehab?
A: I had an obligatory attitude towards my rehabilitation process, since i did not have football as a motivator during my second recovery. I felt that my lack of enthusiasm during this last recovery process hindered the speed of my recovery.
Q: On a scale of 1 -10 how would you rate your adherence to your doctor and therapists recommendations?
A: 2, my lack of motivation was probably the major factor.
Q: What were some of the major milestones during recovery for you?
A: 1) removing the brace 2) being able to lift my hand over my head 3) being able to finally do a push up again
Q: Have you followed your doctors recommendation for exercise since being discharged from PT.
A: No not at all but naturally I exercise and it works my shoulder in the process.